As hospital administrators face growing challenges in retaining nursing and clinical staff, self-scheduling is gaining traction as a promising solution. This approach allows nurses and clinical staff to take greater control over their schedules, promoting a healthier work-life balance that can aid in reducing fatigue and burnout.
The Challenge
Self-scheduling can be an appealing option for health care staff, offering greater autonomy and flexibility in managing work-life balance. However, implementation can be challenging due to the need to ensure adequate shift coverage, fair distribution of work, and a balanced skill mix to maintain patient care quality. Conflicts may arise if staff preferences overlap, leading to understaffed or overburdened shifts, especially on nights, weekends, and holidays. Operational complexities, including cross-department coordination, continuity of care, and overtime, risk further complicate implementation. Additionally, facilities must consider equity concerns, union or policy constraints, and potential resistance from staff or management. Effective self-scheduling often requires significant investment in training and technology, as well as robust conflict resolution mechanisms, to balance autonomy with operational efficiency.
A Ripple Effect
Improving staff satisfaction through self-scheduling, however, can result in significant benefits. When nurses and clinical staff have control over their schedules, unplanned absences and last-minute call-ins may decrease, leading to a more stable and predictable workforce. A satisfied staff not only helps to create a positive work environment, but also translates into improved patient experiences, which foster better patient care and satisfaction. Ultimately, this ripple effect contributes to a stronger reputation and healthier financial bottom line for the facility.
According to the 2024 Nursing Solutions Inc. National Health Care Retention & RN Staffing Report, the average cost of turnover for a bedside registered nurse (RN) has increased by 7.5 percent since 2022, now reaching $56,300 per nurse. This translates to an annual loss of $3.9 to $5.8 million for the average hospital due to RN turnover.
Currently, the average national turnover rate for staff RNs is 18.4 percent. Even a single percentage point change in turnover can significantly affect hospital finances, costing or saving approximately $262,500 per year. These figures underscore the critical importance of introducing new strategies, such as self-scheduling, which enhances retention and reduces turnover.
Case Study: Uncovering the Feasibility of Self-Scheduling
Medecipher, a SnapCare Company, recently conducted an in-depth assessment that highlighted the potential benefits of introducing self-scheduling.
Facility: Suburban Academic Hospital—Level II Emergency Department (ED)
This ED, with an average annual patient visit volume of 43,080, operates on a six-week scheduling period and plans schedules six weeks in advance. The department currently uses a fixed, predetermined grid pattern for scheduling, which stays the same for each cycle. The departmental staff has expressed interest in transitioning to self-scheduling to move away from fixed schedules and gain greater autonomy, but management has been hesitant. Recognizing the importance of improving employee satisfaction, engagement, and retention, the department is exploring whether self-scheduling can be a feasible solution with the following key objectives:
- Providing staff with more flexibility and control over assigned shifts
- Promoting fairness and personalization by eliminating bias or favoritism in shift assignments
- Maintaining a 1:4 staffing ratio to meet patient needs effectively
- Maintaining high compliance with certification rules for ACLS (Advanced Cardiovascular Life Support), BLS (Basic Life Support), PALS (Pediatric Advanced Life Support), TNCC/TNS (Trauma Nurse Core Course/Trauma Nurse Specialist, and ECRN (Emergency Communications Registered Nurse)
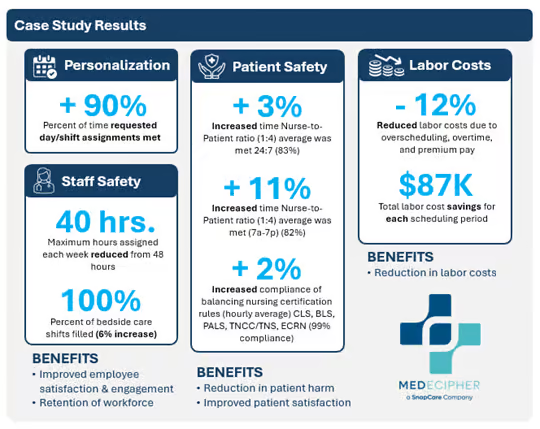
The assessment revealed that innovative technologies like Medecipher’s software can make self-scheduling a viable solution for this ED. The software automatically assigns and balances shifts based on predefined scheduling rules, ensuring a fair and unbiased schedule. This innovative approach not only promotes equity but also enhances staff and patient safety while reducing labor costs.
While the concept of self-scheduling isn’t new, advancements in technology have made implementation more practical and efficient. With nurses and clinical staff increasingly demanding more flexibility and control over their own schedules, self-scheduling is emerging as a powerful tool to meet their needs while maintaining operational efficiency.

