Health care organizations are facing a major new disruption: the recently passed reconciliation bill, H.R. 1. Its potential impact, such as deep Medicaid cuts, stricter eligibility requirements, rising administrative complexity, and shrinking coverage, promises to reshape the health care landscape, especially for providers filling a safety net role in their communities.
As health care organizations prepare for what’s ahead, we find ourselves at a well-known crossroad: the challenge of doing more with less. The central question becomes: How do we continue delivering high-value, safe care in the face of such disruption? But this moment isn’t just about survival—it’s a test of leadership.
Back in 2013, John Toussaint, executive chairman and founder of association corporate affiliate member Catalysis, published “The Promise of Lean in Health Care,” Since, we have observed success and failures in Lean implementations, all while navigating major disruptions like the Affordable Care Act, rapid technological change, and the COVID-19 pandemic.
Why Lean Thinking Matters NOW
With the upcoming disruption, leaders must address the immediate pressures coming from multiple fronts, while maintaining a strategic eye to the future. That’s where Lean comes, and many health care organizations have adopted it with great results, including association members like Zuckerberg San Francisco General Hospital and Trauma Center, in San Francisco, and UMass Memorial Health, in Worcester, Mass. These health systems have demonstrated sustained improvements in cost, quality, access, and patient experience through their long-term commitment to a lean framework. These cases, and additional research, make a strong case for Lean as a strategic approach to both short and long-term success.
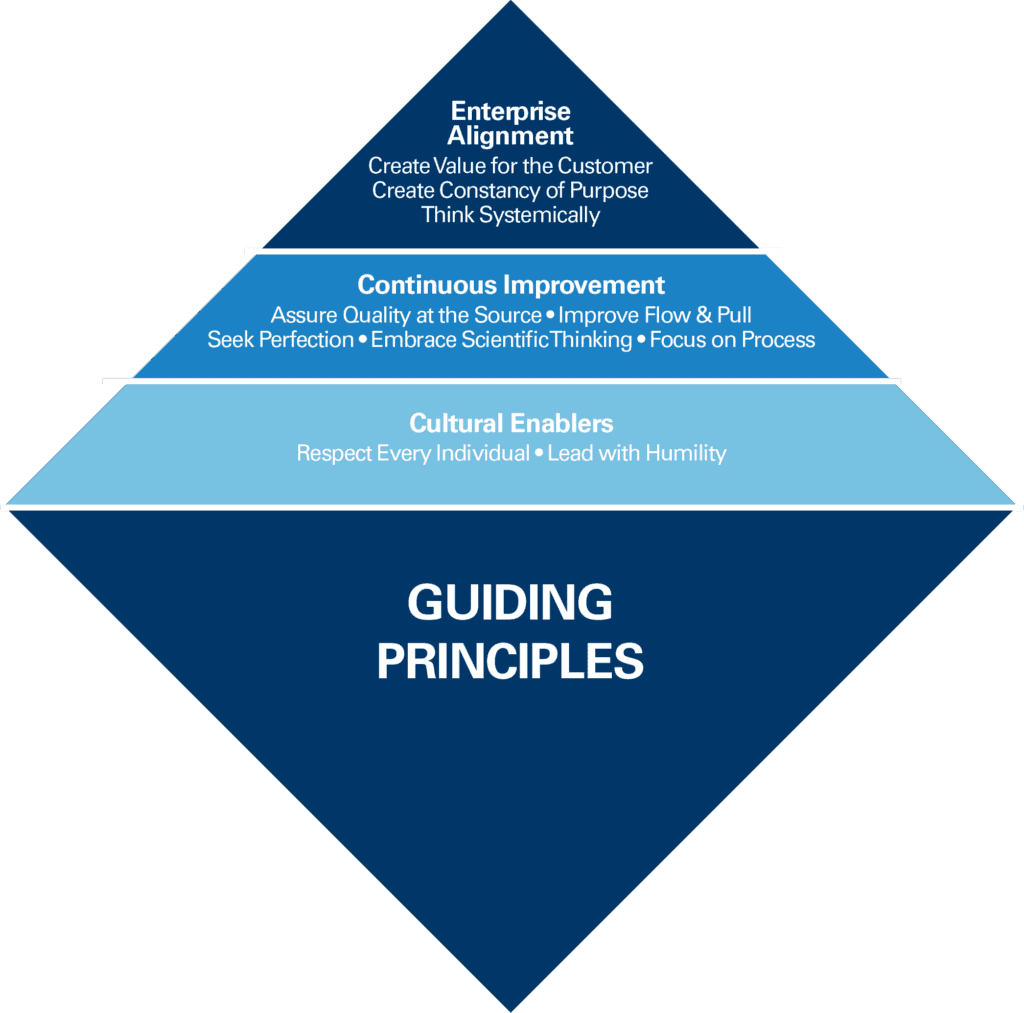
What began as a promise for Lean has become the need for Lean. To meet this moment, organizations must commit to go beyond superficial, tool-based approaches. This requires deep, organization-wide commitment to a principle-based framework, embedded throughout the organization.
How Forward-Thinking Organizations Use Lean Principles in Turbulent Times and Beyond
Enable culture through respect for people and humble leadership
Disruption creates turnover, fear, and burnout. Your ability to retain, engage, align, motivate, and grow people, even in challenging times, will define your resilience. Here’s how:
- Align behaviors with performance at all levels.
- Use leader standard work—simple, consistent daily routines that keep leaders connected to the work, and support coaching, developing, and improving people and processes.
- Cultivate a culture of experimentation and learning through problem-solving,
- Model and reinforce coaching and curiosity: Advise less, ask more, and create psychological safety.
- Develop people relentlessly, not just to perform, but to grow.
Develop an aligned, agile organization through constancy of purpose and systems thinking
A structured and agile strategy deployment system helps teams stay aligned, focused, and adaptable. Here’s how:
- Use Hoshin Kanri to align strategy with daily improvement, maintaining focus on the critical few. This lean strategic planning and management system aligns an organization’s goals and objectives at all levels, focusing on Plan-Do-Study-Act cycles and people development.
- Identify and track measures that matter to patients.
- Design a disciplined strategy execution system across all tiers, maintaining flexibility and adaptability.
- Link strategy to everyday operations with visible goals, rapid problem solving, and front-line engagement, known as a Daily Management System.
Flow and pull value: Redesign care delivery and access
Projected coverage losses could lead to increased emergency department visits, care delays, and uncompensated care. It’s time to rethink care models. Here’s how:
- Leverage Lean Design Methods —such as rapid prototyping of care pathways, value stream mapping of patient journeys, and iterative testing of scheduling workflows—to build integrated care teams and pathways that manage patients with coverage gaps and improve access to care.
- Co-design continuum of care pathways with community partners for timely, appropriate access to resources.
Relentless Continuous Improvement: Seek perfection, focus on the process, assure quality and safety, and embrace scientific thinking
New policies highlight the need to reduce administrative and clinical burden and complexity. Focus on reducing waste without cutting value. Here’s how:
- Use process mapping to identify and eliminate waste in any administrative or clinical workflow
- Apply standardized work and create systems that help maintain and improve it.
- Integrate visual management to reduce human error, improve flow, and enhance clarity.
Integrate AI, technology, and business intelligence through a Lean lens
Artificial intelligence is here—and when used well, it can elevate care delivery, reduce burden, and improve equity. Here’s how:
- Define a purpose-driven AI and business intelligence strategy that enhances human capability instead of replacing it.
- Start with process clarity: map processes and eliminate waste before inserting technology.
- Make AI and business intelligence a core capability.
Final Thoughts
Health care will continue facing financial, regulatory, and operational challenges that will test even the strongest systems. Lean offers much more than tools—it provides a mindset and leadership framework that prioritizes people, enables disciplined action, and builds agile, and resilient teams. Leadership commitment is the greatest success factor. Now is the time for health care executives and improvement leaders to lead with courage, clarity, and purpose and a vision on the future success and sustainability of their organizations. The road ahead is uncertain, but we’re not alone.

